


Context - This is a synthesis which looks at the evolution of cancer rates and its related mortality, as well as at the main types of cancer and the main known causes and prevention means.
This is a faithful synthesis and summary of several scientific consensus reports. For the full list of sources, see the references.
This is a factual synthesis of reports on cancer produced by health organisations worldwide (including WHO1 and the International Agency for Research on Cancer (IARC)2, National Institute of Health (NIH,US) and the US National Cancer Institute3, INSERM4 (France), Cancer Research (UK)5. It highlights the evolution of cancer rates and its related mortality described in these reports, as well as at the main types of cancer and the main known causes and prevention means.
It is important to distinguish between cancer incidence, which reflects the number of cases that are diagnosed, and cancer-related mortality. Because the population is getting older and that age is one of the main risk factors for cancer, the number of cases of cancer is, on the whole, increasing. However, earlier detection and more effective treatments mean that although the number of cases is increasing, the mortality is decreasing, at least for some types of cancer such as breast cancer 6
According to WHO1 the predicted sharp increase in new cases – from 10 million new cases globally in 2000, to 15 million in 2020 - will mainly be due to steadily ageing populations in both developed and developing countries, along with current trends in smoking prevalence and growing adoption of unhealthy lifestyles.
According to the statistics published by the World Health Organisation (WHO)7, in 2012 (latest global statistics available), approximately 14 million new cancer cases were detected and 8.2 million people died from cancers, making it a leading cause of morbidity and mortality worldwide.
The 6 most common types of cancer death identified by WHO are:
Among men, the 5 most common cancers diagnosed in 2012 were lung, prostate, colorectal, stomach, and liver cancer. Among women the 5 most common sites diagnosed were breast, colorectal, lung, cervix, and stomach. In the case of work-related cancers, the most common types are lung cancer, mesothelioma (usually associated with exposure to asbestos) and bladder cancer.
The number of new cases is expected to rise by about 70% over the next 2 decades. According to IARC8 , the estimated future burden of cancer rate worldwide could be much larger than today due to adoption in economically developing countries, of western lifestyles such as smoking, poor diet, physical inactivity, and reproductive factors (age at first menstruation; age at first birth; age at menopause, duration of breastfeeding, the effects of external hormones).
Lung, breast, and colorectal cancers, which are related to these factors, are increasing in economically developing countries. Rates of cancers common in Western countries will continue to rise in these countries if no preventive measures are widely applied.
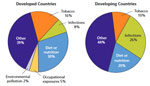
It is usually not possible to know exactly why one person develops a cancer and another doesn’t, but there are known factors that increase a person’s risk of having cancer. About one third of cancer deaths can be linked to five leading risks factors associated with diet and behavior:
As already mentioned, ageing is another fundamental factor for the development of cancer, most likely due to a build up of risks for specific cancers that increase with age, combined with the tendency for cellular DNA repair mechanisms to be less effective as a person grows older.
For WHO, globally 19% of all cancers are also attributable to so-called external “environmental causes”. These include air pollution, exposure to UV radiation, indoor smoke from household use of solid fuels and indoor exposure to radon gas. These represented about 2% of cancer causes in 2008, resulting in 1.3 million deaths each year.
As underlined by WHO9, the roles genes play differ greatly, ranging from genes that completely determine the disease state (disease genes), to genes that interact with other genes and environment factors in causing cancer (susceptibility genes).
In fact, the proportion of cancers directly caused by genetic inheritance is low, about less than 5% for breast cancer, and even less for most other cancer types except retinoblastoma in children.
Studies have shown that indeed the primary determinants of most cancers are lifestyle and environmental factors, rather than inherited genetic factors. However, differences in the way chemical substances are transformed in the body to be eliminated (their “metabolism”), which is genetically controlled, also explain differences in the susceptibility of individuals to cancer.
The WHO10 explains that the transformation from a normal cell to a cancer cell occurs in many steps, usually by a progression from a pre-cancerous lesion to a malignant tumour state. Cells undergo metabolic and behaviour changes that lead them to multiply uncontrollably. These changes can be either mutations to the genes themselves, or to how the genes are expressed in the cell. They are the result of the interaction between a person's genetic factors (family history can be a sign of genetic risk factors) and external agents, such as certain levels of exposure to specific radiation, chemicals or infectious agents.
Any substance that causes cancer is classified as a carcinogen. However, as underlined by the U.S. National Cancer Institute, (NIH)11, just because a substance has been designated as a carcinogen, does not mean that exposure to this substance will necessarily cause cancer. Many factors influence whether a person exposed to a carcinogen will develop cancer, including the amount and duration of the exposure and the individual’s genetic background. Cancers caused by involuntary exposures to environmental carcinogens are most likely to occur in subgroups of the population, such as workers in certain industries who may be exposed to carcinogens on the job.
| Aflatoxins | Coal Tar and Coal-Tar Pitch | Nickel Compounds |
| Aristolochic Acids (from herbs and plants) | Coke-Oven Emissions | Radon |
| Arsenic | Crystalline Silica (respirable size) | Secondhand Tobacco Smoke (Environmental Tobacco Smoke) |
| Asbestos | Erionite | Soot |
| Benzene | Ethylene Oxide | Strong Inorganic Acid Mists Containing Sulfuric Acid |
| Benzidine | Formaldehyde | Thorium |
| Beryllium | Hexavalent Chromium Compounds | Vinyl Chloride |
| 1,3-Butadiene | Indoor Emissions from the Household Combustion of Coal | Wood Dust |
| Cadmium | Mineral Oils: Untreated and Mildly Treated | |
Most cancer risk (and protective) factors are initially identified in epidemiology studies. In these studies, scientists look at large groups of people and compare the risk factors (lifestyle, occupation, …) of those who develop cancer, with those who don’t. These studies may show that the people who develop a certain type of cancer are more or less likely to behave in certain ways or to be exposed to certain substances than those who do not develop it. But, as underlined by the American Cancer Society12, such studies cannot prove on their own that a specific behaviour or substance causes cancer. For example, the finding could be a result of chance, or the true risk factor could be something other than the suspected one. But findings of this type sometimes get attention in the media and can lead to wrong ideas about how cancer starts and spreads. (See the Common Cancer Myths and Misconceptions page provided by the American Cancer Society for more information.)13
Even if a substance or exposure is known or suspected to cause cancer, this does not necessarily mean that it can or should be avoided at all costs. For example, the hormone estrogen that occurs naturally in the body is a known carcinogen. Exposure to ultraviolet (UV) radiation from sunlight is also known to cause cancer (melanoma), but some UV exposure is needed to produce vitamin D and it is neither practical nor advisable to completely avoid the sun.
These substances also include many commonly used medicines, particularly some hormones and drugs used to treat cancer. For example, tamoxifen increases the risk of certain kinds of uterine cancer but can be very useful in treating some breast cancers, which may be more important for some women14.
To reduce exposures to known carcinogens in the workplace, regulations have been put in place worldwide. Outside the workplace, people can also take steps to limit their exposure to known carcinogens, such as testing their basement for the possible presence of radon gas, quitting smoking, limiting sun exposure, or maintaining a healthy weight.
Regarding prevention, there are two main pathways: primary prevention that avoids exposure to risk factors and secondary prevention that favours early detection of cancer through screenings. The first path is the most cost-effective, from a public health standpoint, but the second one is crucial in increasing the survival of people with cancer.
In terms of regulatory classification, the concept of “hazard” refers to the intrinsic properties of an agent (physical, chemical, biological) – its capacity to cause harm - while the concept of “risk” takes also into consideration the probability and extent of exposure to the agent considered as hazardous15.
This may result in different classifications, including for carcinogenic effects, depending on whether risk is integrated as a factor for the classification or not.
The International Agency for Research on Cancer (IARC) classifies substances only in terms of their potential to cause cancer (“hazard or danger”).
More specifically, IARC has evaluated more than 900 agents or processes and these have the classified according to the following scheme16:
| Group | Description | Number |
| (*) low number because in principle IARC evaluates only the substances or processes suspected to be carcinogenic. | ||
| Group 1 | Carcinogenic to humans | 118 agents |
| Group 2A | Probably carcinogenic to humans | 79 |
| Group 2B | Possibly carcinogenic to humans | 290 |
| Group 3 | Not classifiable as to its carcinogenicity to humans | 501 |
| Group 4 | Probably not carcinogenic to humans | 1(*) |
Usually, each country has organizations or agencies that deal with risk management programmes for carcinogens, often in terms of specific types of cancer (e.g. breast, prostate…) or sector (air, water, economical sector). For instance, in Europe, the European Food Safety Authority (EFSA) deals with potential carcinogens associated to food and food production (e.g. pesticides residues).
In the case of workplace exposure, specific lists of substances are also established by agencies like the US or the European Agencies for Safety and Health at Work (OSHA)17, in order to limit exposure to these substances, as well as to other harmful chemicals and agents.

This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!