

Talen:

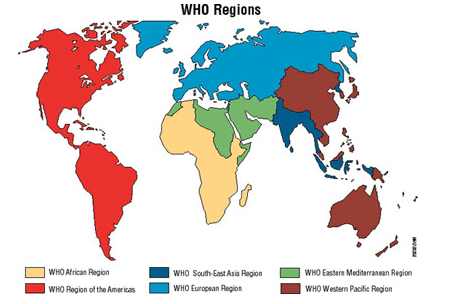

In Africa, the proportion of cases of multidrug-resistant tuberculosis (MDR-TB) is relatively low at 2.2%. It is estimated that in 2006, approximately 67 000 new cases of MDR-TB emerged in the region, with almost 90% of these cases emerging in areas where HIV is widespread.
The lack of adequate laboratory facilities in most African countries makes it very difficult to detect tuberculosis in people who are also infected with HIV. It is also not clear how drug-resistant tuberculosis spreads in areas where HIV infection is common. Given the high rates of HIV infection in some parts of Africa and the lack of laboratories, current figures could underestimate the true burden of MDR-TB in the region.
It is difficult to identify trends of infection in the region as there are only very few surveys available. Preliminary data from Botswana showed that drug resistance is increasing and the results from a further survey will be very important to understand the trends in drug resistance in countries with high rates of HIV. In terms of extensively drug-resistant tuberculosis (XDR-TB), South Africa has recently reviewed its laboratory database and found that 5.6% of multidrug-resistant samples collected over a four year period were in fact extensively drug-resistant. However, these results are not part of a formal survey.
Several countries in the region have nationwide surveys under way or have plans to start them soon, and some of these will include testing for resistance to second-line drugs. Tanzania is evaluating the use of new methods capable of detecting multidrug resistance quickly. If successful, these would be useful to gather information over a wider area and to study trends.
The most critical factor in addressing drug resistance in African countries is the lack of laboratory infrastructure and transport networks that can diagnose drug-resistant tuberculosis quickly. Most countries in the region are far from reaching the targets for multidrug-resistance testing set in The Global Plan to Stop TB 2006-2015. However, there are plans to upgrade national laboratory networks in most countries and to set up at least three new Supra-national Reference Laboratories in addition to the two existing ones.
This text is a summary of: WHO,
![]()
The proportion of drug-resistant tuberculosis among TB cases is low in America as a whole. However, some countries are more heavily affected than others.
In North America, Canada has low proportions of drug-resistant tuberculosis and the number of new cases has decreased every year since 1997. In the USA, tuberculosis is declining and multidrug-resistance even faster.
In South America, there were an estimated 12,070 new cases of MDR-TB in 2006, with Peru alone accounting for about a third of these and Ecuador and Brazil for about an eighth each. This may likely be due to weaknesses in the management of TB cases and in the entire health system in Peru, particularly in the years 2003 and 2004. The proportion of drug-resistant tuberculosis among the general population is low in Argentina, Uruguay and Cuba.
In Brazil and in Mexico there are nationwide surveys under way that test for multidrug-resistance and HIV. A repeat survey in the Dominican Republic is ongoing and Panama also has plans for a nationwide survey.
Currently there are five Supranational Regional Laboratories in the region with plans to expand the network to one or two additional laboratories over the next two years. Many countries have plans to upgrade laboratory networks, and there is more demand for laboratories that can detect resistance to second-line drugs.
This text is a summary of: WHO,
![]()
The information available on drug resistance in the Eastern Mediterranean WHO region has improved significantly since 2002 although it is still limited.
It is difficult to gather information in the region for two reasons. Firstly, many countries are involved in conflicts and struggle to provide even basic health care so they do not have the resources to collect data on drug resistance. Secondly, laboratory infrastructure is poor in many countries of the region.
Approximately 5.4% of all cases of tuberculosis in the region are multidrug-resistant. In 2006 there were approximately 25,000 new cases of multidrug resistant tuberculosis (MDR-TB), and more than half of these were in Pakistan.
The proportion of MDR-TB among new TB cases is low in Morocco, Lebanon and Oman, but higher in Yemen and Jordan. Jordan, Lebanon, and Oman reported very high proportions of resistance among retreated cases, although the results are not very reliable due to small sample sizes.
Currently, there is only one reference laboratory in the region, but two more could be set up. Pakistan has expanded its laboratory services widely and has plans to do a nationwide survey and to start a programme to treat multidrug-resistant tuberculosis. Iran has been planning a second nationwide survey for several years, but has not yet carried it out. Libya, Saudi Arabia and Somalia will start preparation for drug resistance surveys in 2008. Sudan has recently begun a survey.
This text is a summary of: WHO,
![]()
The proportion of cases of tuberculosis that are multidrug-resistant varies widely between Western and Central Europe, where it is only 1.5%, and Eastern Europe and the Central Asian countries, where it is as high as 22.6%.
In most of Western and Central Europe, there is little drug-resistance both in absolute and in relative terms. Israel is an exception and has the highest proportion of resistance in the region. However, most cases of multidrug-resistant tuberculosis (MDR-TB) in Israel were likely to have been infected abroad before immigrating to Israel. Importantly, almost all countries in Western and Central Europe are now linked to a supra-national reference laboratory and the quality of the drug resistance testing and the correctness of the test results are monitored independently.
Countries of Eastern Europe and Central Asia have reported the highest proportions of resistance to anti-tuberculosis drugs in the world and an estimated 80,057 MDR-TB cases emerged in the area in 2006. One of the main factors responsible for this could be the economic crisis that followed the disintegration of the USSR in 1991. This resulted in the deterioration of the health sector and had a devastating effect on the well-being of the population. Other important factors could be the failure of many countries to follow standard procedures to deal with tuberculosis and the spread of drug-resistant tuberculosis in prisons.
In the Baltic countries, the proportion of people diagnosed with TB each year is falling and trends in drug-resistance among new cases appear to be relatively stable. This decline in tuberculosis over the last 10 years is a result of economic growth, investment in health and improved TB control, particularly in Latvia and Estonia, and to a lesser extent in Lithuania. In all three countries, social problems among TB patients, such as alcohol, psychoactive drug abuse and homelessness, have a negative impact on treatment outcomes.
In the Russian Federation, the proportion of people who become ill with tuberculosis is relatively stable and is falling in some areas. In two areas that have provided reliable trend data, However, the number and the proportion of cases that are drug-resistant are increasing considerably despite strong and improving TB control programs, and the reason for this is not clear. While the results from these areas cannot be extrapolated to the country as a whole, they suggest that extraordinary measures will have to be taken if MDR-TB is to be reduced in the population.
Currently, all countries in this sub region are linked to a supra-national regional laboratory with the exception of Turkmenistan and Bulgaria. Several countries are starting or planning national drug resistance surveys. Appropriate MDR TB treatment is becoming available in more and more countries, but additional investment will be needed to meet the targets set out in the Global Plan.
This text is a summary of: WHO,
![]()
The South East Asia WHO region is home to a number of countries that have a high burden of tuberculosis, with India alone accounting for close to two million cases. Though the proportion of cases of multidrug-resistant tuberculosis (MDR-TB) among new TB cases in the region is moderate, the overall number of cases of MDR-TB is considerable. In 2006, approximately 150,000 people became ill with MDR-TB, with three quarters of them living in India.
In five of the six countries that reported data since 2002, the proportion of multidrug resistance among new cases was lower than 3.0% but in Myanmar it was 3.9%, which accounted for over 4000 cases in 2006. Despite these results and the lack of resources, Myanmar has made some progress in TB control.
Levels of drug resistance appear to be moderate in Indonesia, low in Bangladesh and exceptionally low in Sri Lanka where all cases that do not respond to standard treatment are tested for drug-resistance, and multidrug resistance is managed by the public sector. Nepal also shows low levels of drug resistance. .
Recent results from India show low to moderate proportions of multidrug resistance among new cases but considerably higher proportions among those previously treated for tuberculosis. Many such “retreatment” cases are thought to be managed by the private sector and there is concern that, unless the public sector takes up drug-resistance management rapidly, an increasing number of MDR-TB cases will be managed by an unregulated private sector which has access to second-line drugs that are of variable quality. Extensively drug-resistant tuberculosis (XDR-TB) has also been reported in the country.
North Korea could be affected by multidrug-resistance more heavily than other countries in the region. It has developed plans to improve its laboratory capacity to test for resistance but the main obstacle to achieve this goal is lack of sustainable funding.
All countries in the region with the exception of Thailand have identified the upgrading, expansion and quality assurance of their laboratory network as their primary requirement to scale up MDR-TB control.
Unlike the other countries in the region Thailand has an extensive and well developed network of laboratories, some capable of performing tests for resistance to second-line drugs. However, laboratory services are not centralized and many are managed by the private sector, which makes it is difficult to maintain high levels of performance. All MDR-TB patients are managed in the public sector but practices do not follow international guidelines.
This text is a summary of: WHO,
![]()
In 2006, there were over 150,000 new cases of multidrug-resistant tuberculosis (MDR-TB) in the Western Pacific, which represents 6.7% of all cases of tuberculosis in the region. Almost 85% of MDR-TB cases emerged in China. Besides China, the worst affected countries among those that have reported data are Viet Nam and the Philippines.
Data from three provinces in North Eastern China show proportions of multidrug resistance among new TB cases as high as 7.3%, but these are much lower in the cities of Beijing and Shanghai. China has the second highest level of resistance in the world and the extent of resistance to second-line drugs is currently unknown. Although there are plans to expand MDR-TB treatment, China is not on target to meet the goals set for 2011.
Data from Viet Nam suggest that multidrug resistance has not increased over the past 10 years while resistance to any one drug has actually decreased. In 2006, the proportion of MDR-TB was 2.7% among new TB cases but it was much higher among previously treated cases (19, 3 %).
In the Philippines, 4.0% of new TB cases and 20.9% of previously treated cases were MDR-TB in 2004. The Philippines have had a long-running programme to manage multidrug-resistant tuberculosis that is now expanding and is performing well. However, the high proportion of resistance to some second-line drugs and the emergence of extensively drug-resistant tuberculosis (XDR-TB) require careful monitoring.
Trends are available from Hong Kong and South Korea. In both places, the proportion of TB cases in the population has decreased , although it has been relatively stable in the past few years in South Korea. In Hong Kong multidrug resistance has been declining fast, while in South Korea there has been a gradual but significant increase in MDR-TB among new cases.
Available data on XDR-TB show that the highest proportion among MDR-TB is found in Japan followed by Hong Kong. Where absolute numbers of MDR-TB are low, XDR-TB may not represent a significant obstacle for TB control However, in countries with many cases of MDR-TB and widely available second-line drugs, such as China and the Philippines, monitoring of resistance to second-line drugs will be crucial.
China is the only country in the Western Pacific with a significant number of laboratories able to test samples for drug resistance. The region has five very active Supranational Reference Laboratories and there are plans to add one more over the next year. However, to cope with the demand, it may be crucial to forge links with the private sector.
This text is a summary of: WHO,
![]()

This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!