
Sprachen:

The reduction of exposure to harmful chemicals is one of the elements that is put forward among of the Sustainable Development Goals2 : SDG 3, which aims at "Good health and well-being", SDG 12 ("Responsible production and consumption"), which aims specifically to reduce pollution and to better manage waste, and SDG 6, which aims at keeping "clean water and sanitation" by, a.o. reducing pollution, eliminating dumping and minimizing release of hazardous chemicals and materials.

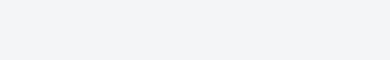
We are indeed exposed to chemicals every day through the food we eat, the air we breathe, the water we drink, what we touch. Many of these chemicals are harmless, but some of them however can be a threat to our health or to the environment. According to the WHO, the known burden due to chemicals is considerable. The increase in the production of chemicals that is projected to continue over the next decades (even to triple in sales by 2050) raises the question of the impact that this could have on public health. Do we know what all of the chemicals that are produced and used, do?
1 Prüss-Ustünet al.: Knowns and unknowns on burden of disease due
to chemicals: a systematic review.Environmental Health 201110:9.
2
www.un.org/sustainabledevelopment/sustainable-development-goals/![]()
To quantify population health impacts from exposure to chemicals, a systematic review of literature compiled the estimates and summaries of chemical exposure and the links between the respective chemicals and disease or injury. In order to measure the impact on human health of any risk factor, be it a disease, exposure to a chemical, or even a lifestyle habit, the World Health Organization (WHO), estimates the number of deaths and the number of healthy life years lost attributed to these particular risk factors. This was expressed in terms of "Disabilty-Adjusted Life Years" or "DALY", which can then be used to evaluate and compare different risk factors3.
Chemicals, whether of natural origin or produced by human activities, are part of our environment.
Their chemical, physical and toxicological properties vary greatly - while many are not hazardous or persistent, some are life-threatening on contact and some can persist in the environment, accumulate in the food chain, travel large distances from where they are released, or are harmful to human health in small amounts.
Humans can be exposed to toxic chemicals through a number of ways, and for each pathway, there are regulatory tools to mitigate that exposure. Air pollutants from ambient and household sources are a mixture of many components including, for example, carbon monoxide (CO), sulfur dioxide (SO2), nitrogen oxides (NOx) and particulate matter, the last containing substances such as acids, organic chemicals, metals, soil and dust particles. For example, pesticides used in agriculture can volatilize and suspend into the air when sprayed.
However, the largest sources of air pollution are combustion and other processes from energy generation, industry and transport. In addition to occupational exposure, inappropriate disposal of building waste can expose the population, and often the poorest communities, to asbestos.
Meanwhile, the presence of naturally occurring hazardous chemicals in food and water can be controlled through the monitoring of the food supply and the decontamination and treatment of water. Occupational, transport, chemical, and product safety mechanisms exist to reduce the amount of harmful chemicals we are exposed to.
3 To better understand the difference between the notions of
hazard and risk in the evaluation of the properties of a chemical see the
short animation video : www.youtube.com/watch?v=PZmNZi8bon8![]()
![]()
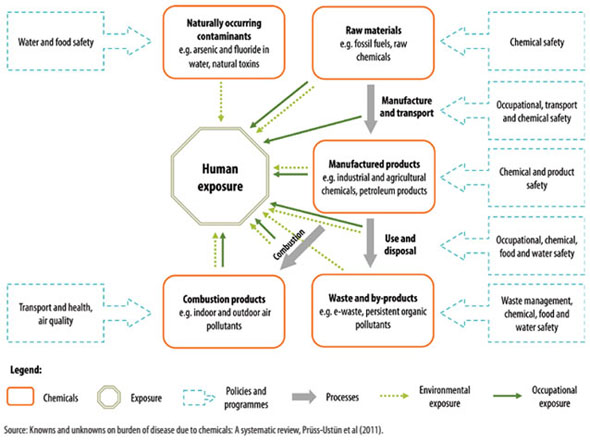
In 2012, 12.6 million deaths globally, representing 23% (95% confidence interval: 13–34%) of all deaths, were attributable to the environment. When accounting for both death and disability, the fraction of the global burden of disease due to the environment is 22% (95% ci: 13–32%).
More specifically, the global burden of disease attributable to environmental exposure and management of selected harmful chemical chemicals amounts to at least 4.9 million deaths (86 million Disabilty-Adjusted Life Year or DALYs4) per year. This represents 8.3% of the total deaths and 5.7% of the total burden of disease in DALYs worldwide.
Exposure to chemicals such as heavy metals, pesticides, solvents, paints, detergents, kerosene, carbon monoxide and drugs lead to unintentional poisonings that are estimated to cause 193 000 deaths annually with the major part being from preventable chemical exposures.
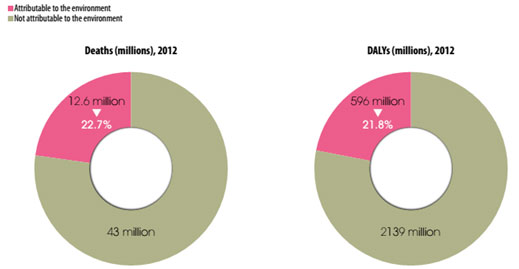
Environmental risks account for up to 26% of all the deaths due to stroke, ischemic heart disease, diarrhea and cancers among children under five.
The environmentally-mediated disease burden is much higher in lower income countries with the exception of certain non-communicable diseases, such as cardiovascular diseases and cancers, where the per capita disease burden is greater in the developed world.
Available information for industrial and agricultural chemicals and acute poisonings only (i.e. without neither air pollution nor arsenic-contaminated drinking-water) amounts to a global burden of disease of at least 1.2 million deaths (25 million DALYs), corresponding to 2.0% of the total deaths and 1.7% of the total burden of disease worldwide.
Nevertheless, WHO considers that the global estimates presented undoubtedly underestimate the real burden attributable to chemicals. It was for example not possible to conduct estimates based on the different modes of action by which chemicals exert their toxic effects, such as through disruption of endocrine, immune, or other systems.
Exposure to chemicals such as heavy metals, pesticides, solvents, paints, detergents, kerosene, carbon monoxide and drugs lead to unintentional poisonings that are estimated to cause 193 000 deaths annually with the major part being from preventable chemical exposures.
4 One DALY can be thought of as one lost year of "healthy" life. The sum of these DALYs across the population, or the burden of disease, can be thought of as a measurement of the gap between current health status and an ideal health situation where the entire population lives to an advanced age, free of disease and disability. (WHO)
There is a long list of chemicals classified with sufficient or limited evidence as human carcinogens. Occupational carcinogens are estimated to cause between 2% and 8% of all cancers. For the general population it is estimated that 14% of lung cancers are attributable to ambient air pollution, 17% to household air pollution, 2% to second-hand smoke and 7% to occupational carcinogens.
Exposure to certain toxic chemicals, such as lead, is associated with reduced neurodevelopment in children and increases the risk for attention deficit disorders and intellectual disability.
Parkinson’s disease has been associated with exposure to some pesticides. Other links between such exposures and mental, behavioral and neurological disorders are suspected; evidence, however, is more limited.
For adverse effects on pregnancy, air pollution and second-hand smoke are specific risk factors with outcomes like low birth weight, prematurity and stillbirths. Exposure to second-hand smoke in the womb for example was estimated to increase by 23% the overall risk for stillbirths and by 13% the risk of congenital malformations. Furthermore, though evidence is limited, there are potential links between exposure to various chemicals and adverse pregnancy outcomes or congenital malformations.
Cataracts are the most important causes of blindness worldwide, and exposure to household cook stove smoke was estimated to be responsible for 35% of cataract disease burden in women and 24% of the overall cataract disease burden.
Second-hand smoke and air pollution are also a contributing factor for 35% of acute lower respiratory infections, including pneumonia, bronchitis and bronchiolitis, the most important cause of mortality in children, and are also linked to upper respiratory infections and ear infections.
More than a third (35%) of overall chronic obstructive pulmonary disease burden is caused by exposure to chemicals in second-hand smoke, air pollution or occupational gases, fumes and dusts. Second-hand smoke and air pollution can induce reduced lung function and a predisposition for pulmonary disease in unborn and young children. Asthma from occupational exposure to asthmagens is among the most frequent disease related to the workplace. More globally, air pollution provokes asthma symptoms exacerbations and increases related hospital admissions.
In the meantime, an expert survey and limited epidemiological data suggest that through restricting access to poisons, about 20% of suicides (over 800 000 individuals die every year) could be prevented. Self-poisoning with pesticides is indeed the main means of suicide in India, China and some Central American countries.
According to the WHO report, about 71% of unintentional poisonings were estimated to be preventable through improved chemical safety. In different sectors, the actions that can be taken vary, but all of them center on better regulating chemicals and pollution. This is something that is sometimes sorely lacking in developing economies, but there is still progress to be made all over the world. While the health sector can directly address certain environmental risks, others are usually managed by other sectors, and inter-sectoral cooperation is essential.
For instance:
Smoking bans in various European and North American countries have reduced exposure to second-hand smoke, and have had a positive impact on health;
The control of industrial emissions, the use of protective measures by workers, changing the way industries deal with dust and dusty environments, all have had a positive effect on the health of workers;
The materials used such as in construction, the way cities are thought out in terms of transportation, the way water supplies are managed, can improve the health of the general population.
WHO indicates that public health can be improved substantially, and in some cases relatively quickly, by identifying and implementing further effective interventions on chemicals of major public health concern. Using measures in all policy areas opens up an additional dimension in public health. Guidance on introducing health in all Policies is available (WHO, 2015).
Social determinants also influence the exposure to and the effect of environmental chemicals, which consequently lead to illness and disease. As these are closely linked to and mediate exposure to environmental risk factors, they need to be systematically integrated into risk monitoring and policy planning in order to reduce health inequalities.
Sectors of particular relevance include energy, transport, industry/commerce, housing and water. In general, modern risks, such as ambient air pollution and unsafe use of chemicals, tend to increase in countries undergoing rapid development, before control over such factors is improved when full transition to high-income societies is made.
Current energy sources – whether fossil fuel, coal or biomass based – which are environmentally unsustainable have negative health consequences. Access to modern fuels for all will end a significant threat to health: exposure to household air pollution resulting from the use of solid fuels for cooking and heating in the household is causing 4.3 million deaths each year. Achieving this goal will have a major impact on health and well-being.
It is also particularly urgent to address those chemicals such as lead and asbestos for which evidence, exposure and policy options have been known for quite some time, international agreements are in place, but exposure and effects are still significant in several populations.
By reducing or removing exposure to chemicals such as from ambient air pollution, household air pollution (in particular from coke stove), second-hand smoke and lead, just over one third (35%) of ischemic heart disease, the leading cause of deaths and disability worldwide, and about 42% of stroke, the second largest contributor to global mortality, could be prevented. For example, in the past, the phase out of leaded gasoline in most countries, provided a powerful example of the impact risk management can have in a relatively short time.
Many environmental risks tend to vary significantly across urban and rural settings. As the world is becoming increasingly urbanized, one key environmental risk in cities is ambient air pollution, causing 3.7 million deaths annually. Air pollution and occupational risks particularly affect the 50 to 70 years age group, in which 25% of all deaths could be avoided through environmental improvements.
Progress on SDG goal 12, which is to ensure sustainable consumption and production patterns and is closely linked to key environmental risks such as ambient air pollution, exposure to chemicals and water and sanitation, would also greatly reduce those risks and protect health.
It is difficult to give an overall, global estimate, but for each sector, specific examples can help grasp the scope of the issue. Overall, prevention of exposure to harmful chemicals seems to be more cost-effective than treatment of the resulting diseases.
Indeed, shifting resources to disease prevention through reducing environmental risks will not only alleviate suffering and increase well-being, but also lead to savings in health care. Some savings are immediate, for example reduced air pollution was shown to have an immediate effect on reducing health care, including emergency visits. When evaluating the costs and benefits of prevention through healthier environments, avoided treatment costs and other externalities caused by unhealthy environments should be accounted for. Shifting resources to disease prevention through reducing environmental risks will not only alleviate suffering and increase well-being, but also lead to savings in health care.
Some savings are immediate, for example reduced air pollution was shown to have an immediate effect on reducing health care, including emergency visits. For instance, in Paraná, Brazil, for each dollar spent on pesticides, approximately US$ 1.28 may be spent on health care and sick leave due to occupational poisoning.
In Hong Kong, the direct and indirect cost of second-hand smoke is estimated at 156 million dollars a year. In the US, the cost of treatment of ischemic heart disease from second-hand smoke is estimated to be between 2 and 6 billion dollars per year. Smoking bans are very cost-effective public health measures.
In the European Union, the economic cost of premature deaths from ambient and household air pollution is estimated to amount to US$ 1.5 trillion in the European Union.
According to the WHO report, the reduction of exposure to harmful chemicals in homes would indeed yield an important financial benefit as well as a reduction in the problems, including in particular some as those related to the overexposure of children to lead, which induces disorders such as attention deficit hyperactivity disorder and would lead to an increase in crime and delinquency.

This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!