

Sprachen:

This GreenFacts synthesis highlights the most recent elements of various reports on cancer prepared by key health organisations worldwide (WHO, IARC, NIH, INSERM, Cancer Research UK, US National Cancer Institute), focusing specifically on:
It is important to distinguish between cancer incidence, which reflects the number of cases that are diagnosed, and cancer-related mortality. The general trends that can be seen in all reports, is that the number of cases in increasing, while mortality is decreasing.
In the EU, between 2004 and 2012 (latest global statistics available), there was a 10.2% decrease in rates of standardized cancer-related mortality in men and a 5.5% reduction in women - see figures 1 (males) and 2 (females) below.
In the US1, the global evolution of cancer rates and deaths between 1930 and 2012 show no overall increase in cancer rates and even a decrease for some major cancers, as well as an overall decrease in cancer deaths. Meanwhile, for some types of cancers, such as melanoma, liver and thyroid the rate is increasing for both men and women.
One trend that is observed in all countries is that there are great differences between cancer types and tumor sites, with some cancers increasing and other decreasing. In the US, for example, pancreatic cancer is expected to surpass breast cancer to become the third leading cause of cancer-related deaths, while in France, a higher frequency of male cancers is significantly correlated with tobacco and alcohol use (lung and upper aerodigestive tract, liver), although for other cancers the trends follow those observed elsewhere.
As reported by INSERM, after adjusting for age rate to reflect the aging of the population, the overall increase in cancer incidence in France between 1980 and 2008 was approximately 35% in men and 43% in women.
The one trend that is observed in all countries is that there are great differences between cancer types and tumor sites, with some cancers increasing and other decreasing.
Regarding mortality rates adjusted for age, there is less regional variability than for incidence, the rates being 15% higher for men in more developed than in less developed regions, and 8% higher in women. In men, the rates are highest in Central and Eastern Europe (173 per 100,000) and lowest in Western Africa (69). In contrast, the highest rates in women are in Melanesia (119) and Eastern Africa (111), and the lowest in Central America (72) and South-Central (65) Asia3.
In France, a slow decrease is observed in women (0.6% annually since 1963), and 1990 (1.6% annually). In men, an increased rate was observed between 1950 and 1980 followed by a decrease of 21% between 1990 and 2004.
According to the World Health Organisation (WHO)2, cancers figure amongst the leading causes of morbidity and mortality worldwide, with approximately 14 million new cases and 8.2 million cancer-related deaths in 2012. The 6 most common causes of cancer death identified by WHO are:
The number of new cases is expected to further rise by about 70% over the next 2 decades from 14 million in 2012 to 22 within the next 2 decades. Further, according to the International Agency for Research on Cancer (IARC)3, more than 60% of world’s total new annual cases occur in Africa, Asia and Central and South America. These regions account for 70% of the world’s cancer deaths. Due to the adoption of western lifestyles, such as smoking, poor diet, physical inactivity, and reproductive factors (age at menarche; age at first birth; parity; age at menopause; and duration of breastfeeding, the effects of exogenous hormones), rates of cancers, which are usually more common in Western, will continue to rise in economically transitioning countries if preventive measures are not widely applied. Among men, the 5 most common sites of cancer diagnosed in 2012 were lung, prostate, colorectum, stomach, and liver cancers. Among women the 5 most common sites diagnosed were breast, colorectum, lung, cervix, and stomach cancers. Regarding occupational cancers, the most common types are lung cancer, mesothelioma, and bladder cancer and one out of ten lung cancer deaths is related to risks in the workplace4.
In the EU, causes of death are classified by Eurostat according to the European shortlist (86 causes, which is based on the International Statistical Classification of Diseases and Related Health Problems (ICD). Chapter II of the ICD covers neoplasms.
The most frequently occurring forms of the disease in the EU are colorectal, breast, prostate and lung cancers. The most frequent cause of cancer death in men is lung cancer, while in women, it is breast cancer. In both men and women, colorectal cancer is the second most common cause of cancer death.
Although significant advances are being made in the fight against the disease, cancer remains a key public health concern and a tremendous burden on European societies.
| % of all deaths from 748cancer | % of total number of deaths. | % of total number of deaths per sex | |
|---|---|---|---|
| Sources: http://eurohealth.ie/2014/11/28/2011-causes-of-cancer-death-in-eu/ www.who.int/mediacentre/factsheets/fs297/en/ |
|||
| lung cancer | 20.7% | 5.4% | 7.5% for men, 3.3% for women |
| colorectal | 11.9% | 3.1% | 3.4% for men and 2.8% for women |
| breast cancer | 7.2% | 1.9% | 3.6% of all death among women |
| prostate cancer | 5.6% | 1.4% | 2.9% of all death among men |
| Tobacco use | around 20% | 70% of global lung cancer deaths | |
| viral infections such as HBV/HCV and HPV | up to 20% | ||
According to the WHO5, around one third of cancer deaths are due to the 5 leading behavioural and dietary risks worldwide: high body mass index, unhealthy diet (low fruit and vegetable intake), lack of physical activity, tobacco use, alcohol use. Among them, tobacco use is the most important risk factor for cancer causing around 20% of global cancer deaths and around 70% of global lung cancer deaths.
According to Cancer Research UK6, smoking, insufficient physical activity, alcohol, diet, overweight, obesity, and infections account for a high proportion of cancers worldwide, as they do in the UK. Cancer risk factors are overall similar worldwide and, even if prevalence of different risk factors varies by region and country, this is partly why overall cancer incidence rates and the most common types of cancer also vary by region and country. The person’s risk of developing cancer depends indeed on many factors, including age, genetics, and exposure to risk factors (including some potentially avoidable lifestyle factors).
Ageing is another fundamental factor for the development of cancer. The incidence of cancer rises dramatically with age, most likely due to a build up of risks for specific cancers that increase with age. The overall risk accumulation is combined with the tendency for cellular repair mechanisms to be less effective as a person grows older. Nine hallmarks of aging have been proposed, including genomic instability and epigenetic alterations, which are also the hallmarks of cancer. 7
As underlined by WHO8, the roles that genes play differ greatly, ranging from genes thcomplete determination of the disease state (disease genes), to interaction with other genes and environment factors in causing cancer (susceptibility genes).
In fact, the proportion of cancers directly caused by genetic inheritance is low, about less than 5% for breast cancer and less for most other cancer types, except retinoblastoma in children.
In particular, family members affected by inherited mutations of the BRCA 1 gene, which accounts for a small proportion of all breast cancers, have a greater than 70% lifetime risk for developing breast or ovarian cancer. However, since the prevalence of germ line mutations such as BRCA1 is very low in most societies, the introduction of mass screening to identify people at risk to develop cancer is not recommended.
Studies have shown that the primary determinants of most cancers are lifestyle and environmental factors rather than inherited genetic factors, but differences in the way people metabolize chemical carcinogens (the so-called metabolic polymorphisms) explain differences in the susceptibility of individuals to cancer. There is a multiplicity of such genetic differences and it seems likely that collectively they explain much of the innate susceptibility to cancer. It may eventually be possible in the future to identify those individuals at special risks such as tobacco- or diet-associated cancers, and also those susceptible to the effects of some environmental contaminants.
WHO 9 explains that the transformation from a normal cell to a cancer cell is a multistage process, typically a progression from a pre-cancerous lesion to a malignant tumour. These changes are the result of interactions between a person's genetic factors and 3 categories of external agents, including:
According to the US National Cancer Institute10, cancer risk factors also include things people cannot control, like age and family history. A family history of certain cancers can be a sign of a possible inherited cancer syndrome. For IARC , cancer is a multi-step process in which cells undergo metabolic and behavioural changes, leading them to proliferate in an excessive and untimely way. These changes arise through modifications in mechanisms that control cell proliferation and lifespan, relationships with neighbouring cells, and capacity to escape recognition and destruction by the immune system.
Modifications that lead to cancer include genetic changes that modify the DNA sequence. Another way to change the programme of cells is to modify the conformation of chromatin, the structure that wraps up DNA and regulates its access by DNA reading, copying and repair machineries. Such changes are called «epigenetic». Among the more than 20 000 genes that constitute the human genome, a few hundred are commonly targeted by genetic or epigenetic changes. These genes are parts of networks of genes that regulate the division, differentiation and life span of cells.
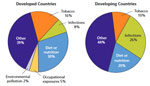
For the WHO, globally, 19% of all cancers attributable to so-called external environmental causes of cancer are factors - defined as any abiotic or biotic element, that influences living organisms and that might bring change to an existing environment - that increase the risk of cancer, and which include air pollution, UV radiation, indoor smoke from household use of solid fuels and indoor radon. These represented about 2% of cancer causes in 2008, including work setting, which results in 1.3 million deaths each year.
For example, in 2004 indoor radon exposure was estimated to cause between 3-14 % of all lung cancers, the second most important cause of lung cancers in many countries. Air pollution caused 165 000 lung cancer deaths globally of which:
Similarly, in 2002, 60 000 deaths were caused by UV radiation of which:
The precise causes of most cancers are not known. As underlined by the National Cancer Institute12, scientists can be more confident about the relationship between a potential risk factor and an increased risk of cancer, when many studies all point to a possible mechanism that could explain how the risk factor could actually cause cancer. Some researchers have suggested that, in most populations, « environmental exposures » (as defined above) are responsible for only a relatively small proportion of total cancers (less than 4 percent), whereas other researchers attribute a higher proportion (19 percent) to such environmental exposures. The substances listed below by the National Cancer Institute are among the most likely carcinogens to affect human health:
| Aflatoxins | Coal Tar and Coal-Tar Pitch | Nickel Compounds |
| Aristolochic Acids | Coke-Oven Emissions | Radon |
| Arsenic | Crystalline Silica (respirable size) | Secondhand Tobacco Smoke (Environmental Tobacco Smoke) |
| Asbestos | Erionite | Soot |
| Benzene | Ethylene Oxide | Strong Inorganic Acid Mists Containing Sulfuric Acid |
| Benzidine | Formaldehyde | Thorium |
| Beryllium | Hexavalent Chromium Compounds | Vinyl Chloride |
| 1,3-Butadiene | Indoor Emissions from the Household Combustion of Coal | Wood Dust |
| Cadmium | Mineral Oils: Untreated and Mildly Treated | |
In parallel, the International Agency for Research on Cancer (IARC) of the WHO has classified 107 agents, mixtures, and exposure situations as carcinogenic to humans28. These include a number of agents found in the environment including:
| All forms of asbestos | Benzene, | Arsenic in water, |
| Cadmium, | Benzo[a]pyrene, | Crystalline silica, |
| Ionizing radiation (including radon and occupational exposure to medical diagnostic imaging), | Non-ionizing radiation (like ultraviolet radiation including tanning devices) | Aluminium production |
| Coke production, | Iron and steel founding, | Rubber manufacturing industry. |
As underlined by the NIH13, any substance that causes cancer is known as a carcinogen, however, because a substance has been designated as a carcinogen does not mean that the substance will necessarily cause cancer. Many factors influence whether a person exposed to a carcinogen will develop cancer or not, including the amount and duration of the exposure and the individual’s genetic background. Cancers caused by involuntary exposures to environmental carcinogens are most likely to occur in subgroups of the population, such as workers in certain industries who may be exposed to carcinogens on the job. According to the US National Cancer Institute14, it is usually not possible to know exactly why one person develops cancer and another doesn’t. But research has shown that certain risk factors may increase a person’s chances of developing cancer. (There are also factors that are linked to a lower risk of cancer. These are sometimes called protective risk factors, or just protective factors). As also underlined by the American Cancer Society15, carcinogens do not cause cancer at all times, under all circumstances. Some may only be carcinogenic if a person is exposed in a certain way (for example, swallowing it as opposed to touching it). Some may only cause cancer in people who have a certain genetic profile. Some of these agents may lead to cancer after only a very limited exposure, while others might require intense exposure over many years. Most cancer risk (and protective) factors are initially identified in epidemiology studies. In these studies, scientists look at large groups of people and compare those who developed cancer with those who didn’t. These studies may show that the people who developed cancer are more or less likely to behave in certain ways or to be exposed to certain substances than those who do not develop cancer.
Such studies on their own, cannot prove that a behaviour or a substance causes cancer. For example, the finding could be a result of chance, or the true risk factor could be different from the suspected one. But findings of this type sometimes get attention in the media, and this can lead to erroneous ideas about how cancer starts and spreads. (See the Common Cancer Myths and Misconceptions page provided by the American Cancer Society for more information.)16
Even if a substance or exposure is known or suspected to cause cancer, this does not necessarily mean that it can or should be avoided at all costs, states the American Cancer Society. For example, estrogens that occurs naturally in the body are known carcinogens. Exposure to ultraviolet (UV) radiation from sunlight is also known to cause cancer, but it is not practical (or advisable) to completely avoid the sun. These lists also include many commonly used medicines, particularly some hormones and drugs used to treat cancer. For example, tamoxifen increases the risk of certain kinds of uterine cancers but can be very useful in treating some breast cancers, which may be more important for some women17. Regulations have been put in place worldwide to reduce exposures to known carcinogens in the workplace. Outside the workplace, people can also take steps to limit their exposure to known carcinogens, such as quitting smoking, limiting sun exposure, maintaining a healthy weight, or testing their basement for radon.
For the WHO , by modifying or avoiding key cancer risk factors, more than 30% of cancer deaths could be prevented.
For the National Cancer Institute , people can avoid some cancer-causing exposures, such as tobacco smoke and the sun’s rays. But others are harder to avoid, especially if they are in the air we breathe, the water we drink, the food we eat, or the materials we use to do our jobs. Scientists are studying which exposures may cause or contribute to the development of cancer. Understanding which exposures are harmful and where they are found, may help people to avoid them.
For Eurostats, primary prevention offers the most cost-effective, long-term strategy for reducing the European burden of diseases. It involves tackling major health determinants, such as smoking, unhealthy diets and physical inactivity. The European Commission has supported many projects related to health determinants and health promotion in general.
For WHO18, early diagnosis is particularly relevant when there are no effective screening methods, or – as in many low-resource settings– no screening and/or treatment interventions implemented. Screening programmes are especially effective for frequent cancer types for which cost-effective, affordable, acceptable and accessible screening tests are available to the majority of the population at risk. In 2014, a report to the European Commission noted that the number of adults surviving for at least five years after diagnosis has risen steadily over time across the EU, thus reflecting major advances in cancer management such as organised cancer screening programmes and improved treatments.
In the EU, a first Council Recommendation on cancer screening was adopted in December 2003, setting out principles of best practice in the early detection of cancer, and a second report on the implementation of the Council Recommendation was adopted in September 201419 . This invited EU Member States to take common action to implement national population-based screening programmes for breast, cervical and colorectal cancer, with appropriate quality assurance at all levels.
In terms of regulatory classification, “hazard” refers to the intrinsic properties of an agent (physical, chemical, biological) – its capacity to cause harm - while “risk” takes also into consideration the probability and extent of exposure to the agent considered as hazardous20 . This may result in different classifications, including for carcinogenic effects, depending on the integration or not of the risk as a factor for the classification.
The International Agency for Research on Cancer (IARC), the cancer agency of the World Health Organization, produces science-based reports and develops since 1971 lists of substances that, based on the available scientific evidence, are known or are reasonably anticipated to be human carcinogens or that can increase the risk of cancer in humans. Their classification is based on the intrinsic carcinogenic hazard potential and not on the real risk; indeed IARC states that the probability of developing a cancer will depend on factors such as the type and extent of exposure, and the strength of the effect of the agent21. More specifically, IARC has evaluated more than 900 agents, including chemicals, complex mixtures, occupational exposures, physical agents, biological agents, and lifestyle factors. Of these, more than 400 have been identified as carcinogenic, probably carcinogenic, or possibly carcinogenic to humans. To this end, IARC convenes expert scientists to evaluate the evidence that an agent can cause cancer. The agency describes the principles, procedures, and scientific criteria that guide the evaluations. Agents are selected for review based on two main criteria: (a) there is evidence of human exposure and (b) there is some evidence or suspicion of carcinogenicity.
The substances are the classified according to the following scheme :
| (*) low number because IARC evaluates only the susbtances or processes suspected to be carcinogenic | ||
| Group 1 | Carcinogenic to humans | 118 agents |
| Group 2A | Probably carcinogenic to humans | 79 |
| Group 2B | Possibly carcinogenic to humans | 290 |
| Group 3 | Not classifiable as to its carcinogenicity to humans | 501 |
| Group 4 | Probably not carcinogenic to humans | 1(*) |
In the U.S., the National Toxicology Program (NTP), an interagency program of the U.S. Department of Health and Human Services (HHS) publishes the Report on Carcinogens every few years. This congressionally mandated publication identifies agents, substances, mixtures, or exposures (collectively called “substances”), in the environment that may cause cancer in humans. The 2014 edition listed 56 known human carcinogens and included descriptions of the process for preparing the science-based report and the criteria used to list a substance as a carcinogen23. Further, Standards for carcinogens are addressed by the Occupational Safety and Health Administration’s (OSHA) in specific standards for general industry, shipyard employment, the construction industry, and the identification, classification, and regulation of carcinogens that apply to substances that are classified as carcinogens or potential carcinogens by the NTP.
The Globally Harmonized System of Classification and Labelling of Chemicals (GHS) now also classifies carcinogens. This United Nations initiative aims at harmonizing the various existing systems of classification of chemical risks worldwide. The GHS is based on the three classification systems already existing in Europe, USA and Canada and on the UN's Recommendations on the Transport of Dangerous Goods. The new regulation will repeal the existing Dangerous Substances Directives 67/548/EEC and 1999/45/EC. It classifies carcinogens into two categories of which the first may be divided again into subcategories if so desired by the competent regulatory authority.

In the EU, the Law on Classification, Labelling and Packaging (CLP or CLaP) is the version of GHS that has been introduced in the EU. CLP complies with the old classification system even if some of its parts have been modified. CLP is binding in all member states and entered into effect on 20 January 2009, with a transitional period that ended June 2015. Regarding carcinogens, it consists of three categories:
Further, other authorities like the European Food Safety Authority (EFSA) also evaluates substances, like pesticides regarding the risk of cancer to exposed populations.
In the case of workplace exposure,
specific lists of substances are also established by agencies like the
US or the European Agencies for Safety and
Health at Work (OSHA), so as to
limit exposure to these substances as well as to other harmful chemicals
and other agents. Among others, the U.S. National Institute for
Occupational Safety and Health (NIOSH) cover
carcinogens in relation to
occupational exposures and publish
specific lists. www.cdc.gov/niosh/topics/cancer/npotocca.html![]()
Other national institutions, such as the Canadian
Centre for
Occupational Health and
Safety also cover the agents specifically related to
occupational exposures and publishes
a list of examples of occupations and occupational groups that are more
likely to have been exposed to
carcinogens are listed in
the following table. This list was complied from information available
from reputable sources, but it is not complete. It represents
associations that have been reported in literature between occupations
and examples of substances often linked to
cancers that may have been used
in the workplace.
www.ccohs.ca/oshanswers/diseases/carcinogen_occupation.html![]()
Other national institutions such as Cancer Research UK24 or the NIOSH25 in the US, the Federal Institute for Occupational Safety and Health (BAuA)26 in Germany also develop evaluation systems of potentially carcinogenic agents, for example more specifically related to occupational exposures.
In Japan, for example, the Industrial Safety and Health Law (ISHL) implemented in 197227 regulates chemicals used in workplace with the purpose of preventing workers from exposure to carcinogens.
www.cancer.gov/about-cancer/causes-prevention/risk/hormones![]()
U.S. National Cancer Institute
at the National Institutes of
Health
Estrogens, a group of female sex hormones, are known human carcinogens. Although these hormones have essential physiological roles in both females and males, they have also been associated with an increased risk of certain cancers. For instance, taking combined menopausal hormone therapy (estrogen plus progestin, which is a synthetic version of the female hormone progesterone) can increase a woman’s risk of breast cancer. Menopausal hormone therapy with estrogen alone increases the risk of endometrial cancer and is used only in women who have had hysterectomy.
Studies have also shown that a woman’s risk of breast cancer is related to the estrogen and progesterone made by her ovaries (known as endogenous estrogen and progesterone). Being exposed for a long time and/or to high levels of these hormones has been linked to an increased risk of breast cancer. Increases in exposure can be caused by: starting menstruation early, going through menopause late, being older at first pregnancy, and never having given birth. Conversely, having given birth is a protective factor for breast cancer.
Diethylstilbestrol (DES) is a form of estrogen that was given to some pregnant women in the United States between 1940 and 1971 to prevent miscarriages, premature labor, and related problems with pregnancy. Women who took DES during pregnancy have an increased risk of breast cancer. Their daughters have an increased risk of a cancer of the vagina or cervix. The possible effects on the sons and grandchildren of women who took DES during pregnancy are being studied.
Radiation
www.cancer.gov/about-cancer/causes-prevention/risk/radiation![]()
U.S. National Cancer Institute at the National Institutes of Health
Radiation of certain wavelengths, called ionizing radiation, has enough energy to damage DNA and cause cancer. Ionizing radiation includes radon, x-rays, gamma rays, and other forms of high-energy radiation. Lower-energy, non-ionizing forms of radiation, such as visible light and the energy from cell phones and electromagnetic fields, do not damage DNA and have not been found to cause cancer.
Radon
Radon is a radioactive gas given off by rocks and soil. Radon is formed when the radioactive element radium breaks down. Radium in turn is formed when the radioactive elements uranium and thorium break down. People who are exposed to high levels of radon have an increased risk of lung cancer.
If you live in an area of the country that has high levels of radon in its rocks and soil, you may wish to test your home for this gas. Home radon tests are easy to use and do not cost much. There are many ways to lessen the amount of radon in a home to a safe level. For more information on radon, see the Radon page and the Radon and Cancer fact sheet.
X-Rays and Other Sources of Radiation
High-energy radiation, such as x-rays, gamma rays, alpha particles, beta particles, and neutrons, can damage DNA and cause cancer. These forms of radiation can be released in accidents at nuclear power plants and when atomic weapons are made, tested, or used.
Certain medical procedures such as chest x-rays, computed tomography (CT) scans, positron emission tomography (PET) scans, and radiation therapy can also cause cell damages that lead to cancer. However, the risks of cancer from these medical procedures are very small, and the benefit from having them is almost always greater than the risks.
1 American Cancer Society. ![]()
2
WHO Fact sheet N°297 Updated February 2015![]()
3
![]()
and http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx![]()
see also : and See also IARC press release - Latest cancer
statistics : ![]()
4
![]()
5
www.who.int/mediacentre/factsheets/fs350/en/![]()
6
www.cancerresearchuk.org/health-professional/cancer-statistics/worldwide-cancer#heading-Two![]()
7
Age and Cancer Risk A Potentially Modifiable Relationship![]()
8
www.who.int/genomics/public/geneticdiseases/en/index3.html![]()
9
WHO Fact sheet N°297 Updated February 2015![]()
10
www.cancer.gov/about-cancer/causes-prevention/ris![]()
11
![]()
12
www.cancer.gov/about-cancer/causes-prevention/risk![]()
13
www.cancer.gov/about-cancer/causes-prevention/risk/substances/carcinogens![]()
14
www.cancer.gov/about-cancer/causes-prevention/risk![]()
15
www.cancer.org/cancer/cancercauses/othercarcinogens/generalinformationaboutcarcinogens/known-and-probable-human-carcinogens![]()
16
www.cancer.org/cancer/cancercauses/othercarcinogens/generalinformationaboutcarcinogens/known-and-probable-human-carcinogens![]()
17
www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-treating-hormone-therapy![]()
18
www.who.int/mediacentre/factsheets/fs297/en/![]()
19
![]()
20
See the short GreenFacts video on the subject:![]()
21
![]()
22
http://monographs.iarc.fr/ENG/Classification/![]()
23
www.cancer.gov/about-cancer/causes-prevention/risk/substances/carcinogens![]()
24
www.cancerresearchuk.org/health-professional/cancer-statistics/worldwide-cancer#heading-Two![]()
25
www.cdc.gov/niosh/topics/cancer/npotocca.html![]()
26
www.baua.de/en/Topics-from-A-to-Z/Hazardous-Substances/Workshops/DMEL-2011/pdf/DMEL-2011-02.pdf?__blob=publicationFile&v=2![]()
27
www.cirs-reach.com/Japan_CSCL/Japanese_Existing_and_Notified_Chemical_Substances_Inventory_ENCS.html![]()
28
![]()

This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!